By Chrys Collins, RN, MSN Ed, CRRN
Photos given with permission by interviewees

We have now come to the conclusion of this series. Let’s hear what wisdom Brittany and Venus have to add to the conversation.
When I interviewed Brittany Brown, a few other questions were added. I asked more because Brittany is considering another child, and I wondered if these thoughts were at the forefront of her mind because of the potential of another baby.
These questions included the following:
1. If you were to have another child would you choose a hospital birth or a birth center birth? Why or why not?
2. Were there any things surrounding delivery and postpartum you wish you had done differently?
MEET BRITTANY
Brittany was able to detail moments from her first labor that were the least supportive, including her feeling as though the doctor was not patient and was “ready to do a c-section”. Her perception was that he was not willing to wait for the natural birth process to take place.
The highlight of that moment, though, came when “the nurse stepped in and said we are pushing.” Brittany credits a successful delivery to a nurse who was willing to advocate for her.
Brittany added that she was determined to breastfeed but found it almost overwhelming. She was thankful for the encouragement and the help of staff willing to reassure her which led to better success.
Brittany found herself pregnant again very quickly after the birth of her first child. Here her response to my question regarding doing things differently was wishing for more birth control discussion.
Although delighted to be a momma of two, the thought of having two babies under two was daunting. For her second birth, Brittany was especially appreciative that a physician took the time before delivery to discuss birth control options for after the baby came.
With the birth of her second child Brittany recalls feeling overwhelmed by the thought of going home and getting little sleep. Because she was breastfeeding, she was met by the nursing staff with resistance to allow the baby to stay in the nursery for her last night in the hospital. She remembers thinking, “I just want one night’s sleep before I go home with two small children.”
Brittany had the support of loved ones who were willing to help advocate for her needs and the baby stayed in the nursery allowing her the night’s sleep she felt she needed.
Sadly, Brittany also felt she dealt with some unaddressed postpartum depression that she believed could have been best dealt with if she’d been given the opportunity to fill out a screening questionnaire.
Despite some drawbacks, Brittany said she would “do it all again in a heartbeat”.
MEET VENUS
Last, but definitely not least, is Venus.
Venus has had three children, all hospital births.
Venus felt her needs were no different than any other woman and was especially thankful for nurses who were attentive to both her physiological and psychological needs.
She mentioned her most recent birth in which nurses made sure all night that her oxygen levels stayed where they needed to be as well as made her feel well cared for during and post-delivery.
Venus also recounted a terrible miscarriage she suffered in 2008 that led to some deep fears in her subsequent pregnancy.
Doctors and nurses from the practice that she attended checked in with her emotionally, offering a place “to vent if needed and to make sure she was ok” by not only helping her with her mental health but reminding her to eat and sleep well. Her care provider made provision during the labor and delivery to ensure that her support system made it to the delivery on time.
Venus seriously considered a birth center or home birth delivery for her last delivery. Despite home birth and birth center birth being more than $6,000 less than a hospital birth, neither of her insurances would cover the birth of her choice.
However, she was given the opportunity to experience a more “natural hospital birth”, stating, “The staff made sure I had a tub, birth ball, and peanut pillow.”
One particularly fond memory Venus had was of a nurse who left her telephone number with her because she was having some challenges breastfeeding her baby. Venus added that she knew that other women may not have had the experience that she did, however she was “blessed to have loving and caring nurses”.
Because of her desires and research, she ended our interview urging women to have their babies at a birth center if they could.
CONCLUSION
The number of women I spoke with was very small and by no means a reflection of the population. Their experiences and outcomes were mostly positive. Looking back at their stories, what do you think they had in common with each other?
As I listened, I heard safety. They each had specific needs that were met physically, emotionally and even perhaps spiritually.
Each woman had the support of people who advocated for her. To me it also seems that each woman was an active participant in her care giving her power and autonomy.
My own experience as a patient and a white woman affirms that there are still obstacles and challenges that must be addressed in medicine.
I have about a half dozen “theories” regarding the disparities that exist with the current outcomes for Black women and their babies. These ideas include epigenetic factors, genetic factors, racism, bias, and fear that could lend to the problem.2 But I feel discussing those things would be more than a blog series, and I am no expert.
I can tell you what I do know, and that is that every woman has basic needs. Meeting those needs can be the very thing that makes a difference in outcomes. I firmly believe this because I have seen it, and literature supports better outcomes when those being cared for are cared for holistically.
Katharine Kolcaba is a nurse theorist who developed a nursing theory called The Comfort Theory that suggests that comfort exists in three forms: relief, ease and transcendence.1
If specific patient needs are met, the patient experiences relief. Relief then gives way to varying degrees of ease and contentment. Ease and contentment then lead to transcendence, which is a state in which a patient is able to rise above the challenges they face. Kolcaba’s theory applies the forms of comfort to four contextual areas: physical, psychospiritual, environmental and sociocultural.1
Remember I said I’d come back to Ayana?
I suspect Ayana is a positive woman by nature. However, I would also like to believe that her ability to reach acceptance of some of the unwanted aspects surrounding her delivery are a prime example of The Comfort Theory in action. Ayana’s physical, emotional, social, and environmental needs were met. She quickly transitioned and was able to adapt and take on the next challenge.
If you have had a baby in the past 20 years in the hospital you may recall that you were not allowed to eat or drink. You had your ration of ice chips and you hoarded them. They were all yours and no one could have them! I was so hungry with my first birth that I think my ice chips may have actually tasted like chocolate.
So now I have a question for you: Why do you think food and drink is withheld from a woman in labor? (Cue Jeopardy music in the background.)
Ready for the answer?
The practice originated in the 1950s when respirator tubes did not have balloons to seal the airway and protect it should a woman need anesthesia for a cesarean section and vomit while under sedation. Since then, respirator tubes are now made with balloons to protect the airway.
It might also surprise you to know that vomiting in the event of being put to sleep is not common.
And, finally there is far more evidence to support giving a laboring woman food and drink than withholding it.3
I brought that up because modern obstetric practices include examples like the one above that have little or no research to support them. Again, I believe there is a time and place where intervention is needed. Healthy, uncomplicated pregnancy and delivery does not need to be included.
I can’t help but feel a little pride when considering what the midwifery model of care offers. Midwifery care uses evidence-based practices supported by up-to-date research. It is gentle and patient. Midwives advocate for their patients not only through the model but in the event that a woman must transfer to a hospital, the midwife is there with her.
Midwifery offers natural birth and hands-on support during the labor process.
Midwives are able to provide comfort and ease and help women through the challenges to take on the next hurdle.
Midwifery offers personalized care to the whole family. This care supports the unique needs of each person. Remember when Brittany felt as though her depression was not addressed? In part that may have been because it is hard to get to know a woman in a 15 minute time segment for her prenatal appointments.
Our own birth center sets aside a one-hour time slot for each appointment. I personally think that gives the midwife time to really get to know her patients. Additionally, more time spent allows for a higher degree of patient trust and I believe more willingness on behalf of the patient to confide in the care provider.
Our birth center has a form with screening questions for the home visit that takes place 24-36 hours after delivery. Don’t forget Tameka from Part One. A visit just like this could have saved both her and her baby.
Moms are also encouraged to come back at week one and two for a baby weight check. This allows for additional wellness assessments for mom and baby.
Forgive me for my bias. I know I’ve talked a lot about midwifery and even some about our birth center, which is near and dear to my heart. I also know not everyone is a midwife or can be taken care of by one. It just seems to me that almost everything our women needed in their stories, even in Tameka’s story, the midwifery model provides.
If nothing else, the extra time midwives give to patients meets many women’s needs organically.
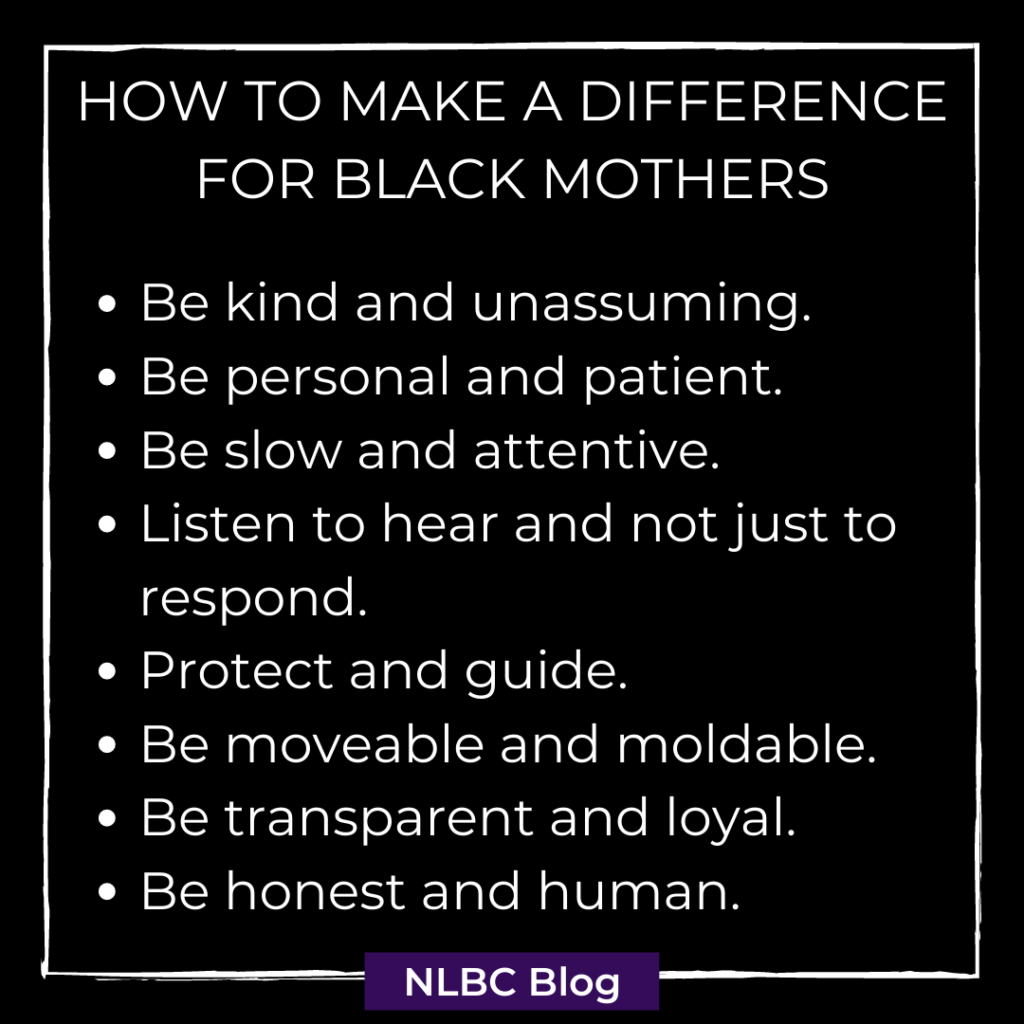
Perhaps to make a difference we can adopt just a few takeaways from the ladies in our interview and the midwifery model of care.
How to Make a Difference for Black Mothers:
- Be kind and unassuming.
- Be personal and patient.
- Be slow and attentive.
- Listen to hear and not just to respond.
- Protect and guide.
- Be movemeable and moldable.
- Be transparent and loyal.
- Be honest and human.
These points are good advice for all areas of our lives. For health care providers, for communities, for anyone across any “divide”- whether between provider and patient, male and female, or any two people with ethnic or cultural differences. This is the way we love our neighbor. This is the way we can truly make a difference.
References:
1Kolcaba, K. (2019). The Comfort Line. Comfort Line. https://www.thecomfortline.com/
3Dekker, R. (2021, February). Evidence on: Eating and Drinking During Labor. Evidence Based Birth. https://evidencebasedbirth.com/evidence-eating-drinking-labor/



[…] A Call to Make a Difference for Black Mothers: PART FOUR – New Life Birth Center | Roanoke Valley Mi… says: March 19, 2021 at 1:06 pm […]